DECEMBER 2, 2024
Allergen Avoidance | Symptomatic
Treatment | Desensitization
3 Allergic Rhinitis Management Options

There are 3 general management approaches to allergic rhinitis (AR):
Which one(s) you choose for your patient depends on many factors, including patient characteristics, severity, success with previous therapies, safety/tolerability, and patient preference.
Allergen Avoidance
First-line AR management involves identifying and avoiding allergens that trigger symptoms. This may mean recommending that your patient make changes to their environment and/or lifestyle.
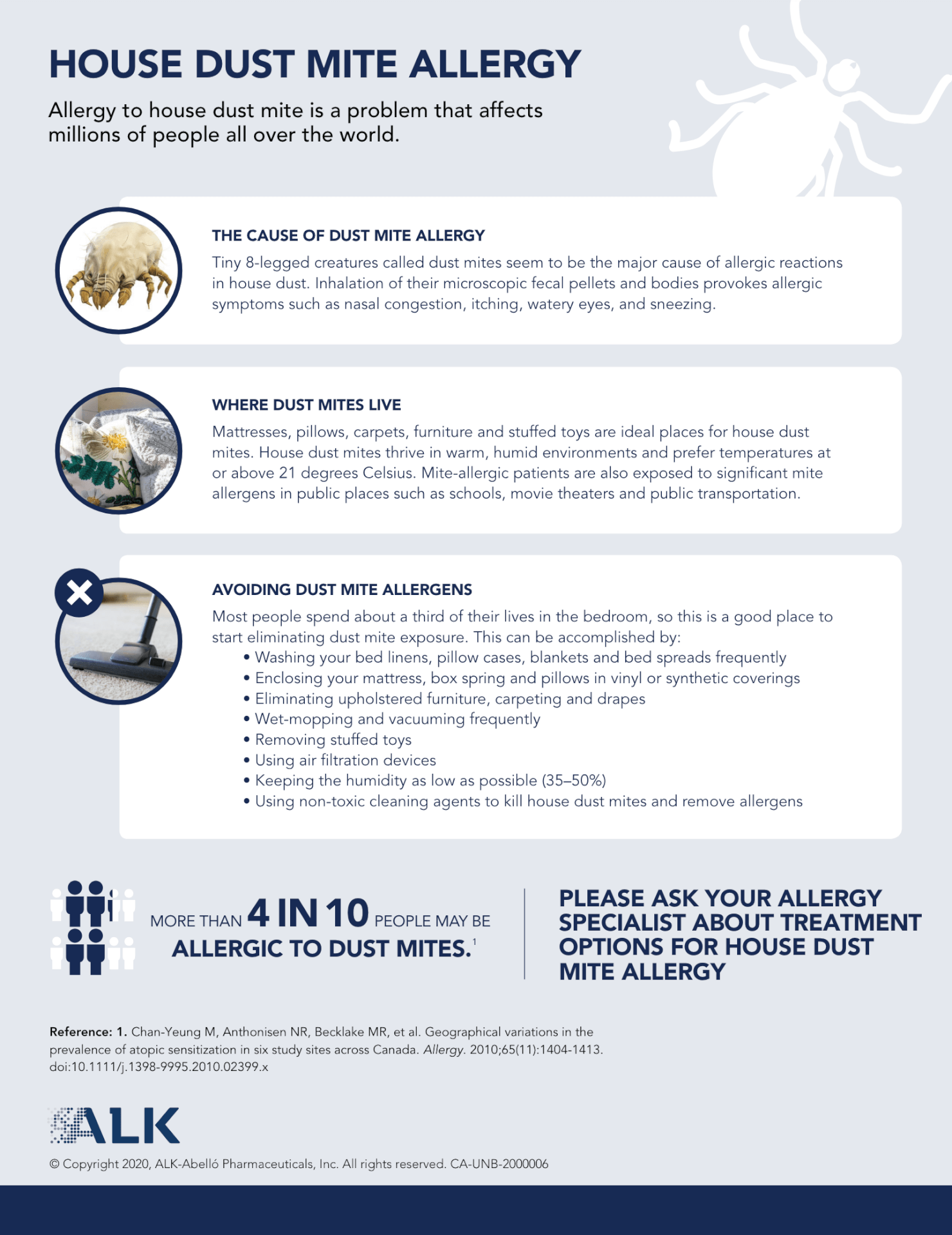
For example, if pollen is a trigger, patients are usually advised to avoid spending time outdoors during peak pollen seasons, keep windows closed, and use window screen filters and air conditioners. Similarly, if patients are allergic to dust mites, cleaning practices like regular vacuuming, washing bedding in hot water, and removing carpets can be beneficial.

Avoidance can significantly reduce exposure to allergens and reduce symptoms, but it isn’t always practical (think: construction labourer, arborist, or housekeeper), and sometimes it can be difficult to pinpoint the cause(s) of symptoms.
Download the House Dust Mite (HDM) Allergy Information Sheet to share helpful tips with your patients on managing HDM allergy
Symptomatic Treatment
When avoidance is not enough or not feasible, symptomatic treatment is usually the next step. This approach focuses on managing symptoms of allergic rhinitis through over-the-counter or prescription medications. There are several types of medications available, including:

Second-generation* oral antihistamines:
Antihistamines block histamine to help relieve allergy symptoms. These drugs have been shown to effectively relieve sneezing, itching, and rhinorrhea when taken as needed.
Intranasal corticosteroids:
These medications are also recommended first-line for patients with mild persistent or moderate/severe symptoms and can be used alone or in combination with oral antihistamines. When used regularly and correctly (patient counselling is necessary to ensure proper application and to help avoid local side effects), they can reduce inflammation in the nasal passages and effectively relieve symptoms like nasal congestion, itching, and sneezing. Nasal corticosteroids are typically used long-term.


Leukotriene receptor antagonists (LTRAs):
LTRAs block leukotrienes from causing AR symptoms. Generally, LTRAs do not appear to be as effective as intranasal corticosteroids and should only be considered if intranasal corticosteroids are ineffective or not well tolerated. There is currently only one LTRA indicated in adults for AR in Canada.
Desensitization (Allergy Immunotherapy [AIT])
AIT works to address the root cause of allergic rhinitis, which is triggered by abnormal immune responses to specific allergens. Patient-specific allergens are introduced in small, controlled doses under medical supervision to induce immunologic tolerance. It is the only disease-modifying therapy for allergic rhinitis.
AIT is administered to patients as sublingual tablets or subcutaneous injections. The sublingual tablets are taken daily with standardized dosing. The subcutaneous route involves weekly injections with gradual dose increase over a period of time until reaching the effective maintenance dose.
The sublingual immunotherapy tablets (SLIT-t) are offered for the most prevalent allergens in Canada, including HDM, birch/alder/hazel tree, grass, and ragweed. The subcutaneous immunotherapy(SCIT) can be used for those allergic to many different kinds of environmental allergens. Patients must undergo skin prick testing or specific IgE testing to identify their allergen(s) before being prescribed AIT.
AIT is usually recommended when avoidance and symptom relievers are either suboptimal or not well tolerated.
Looking for more AIT information for your patients?
We can help!

Other approaches to AR management
Other approaches to managing AR symptoms may include oral and intranasal decongestants, intranasal sodium cromoglycate, and in rare cases, surgery; however, these are not commonly used. Complementary and alternative medicines (CAM) are generally not recommended due to the lack of high-quality studies supporting their use.
* First-generation sedating antihistamines, while effective, are no longer routinely recommended due to their impact on cognition and functioning.
